Observation Unit Pandemic Operation 2020, A National Survey by the ACPAAnthony Joseph, MD; Amit Wadhwa, MD; Anuja Mohla, MD; Bartho Caponi, MD; Robert Tano, MD; Russell Firman, MD; Steven Meyerson, MD; Bernard H. Ravitz, MD Observation Services have become increasingly important for patients who benefit from hospitalization for a short period of time beyond the Emergency Department. Two major approaches to the care of these patients has emerged:
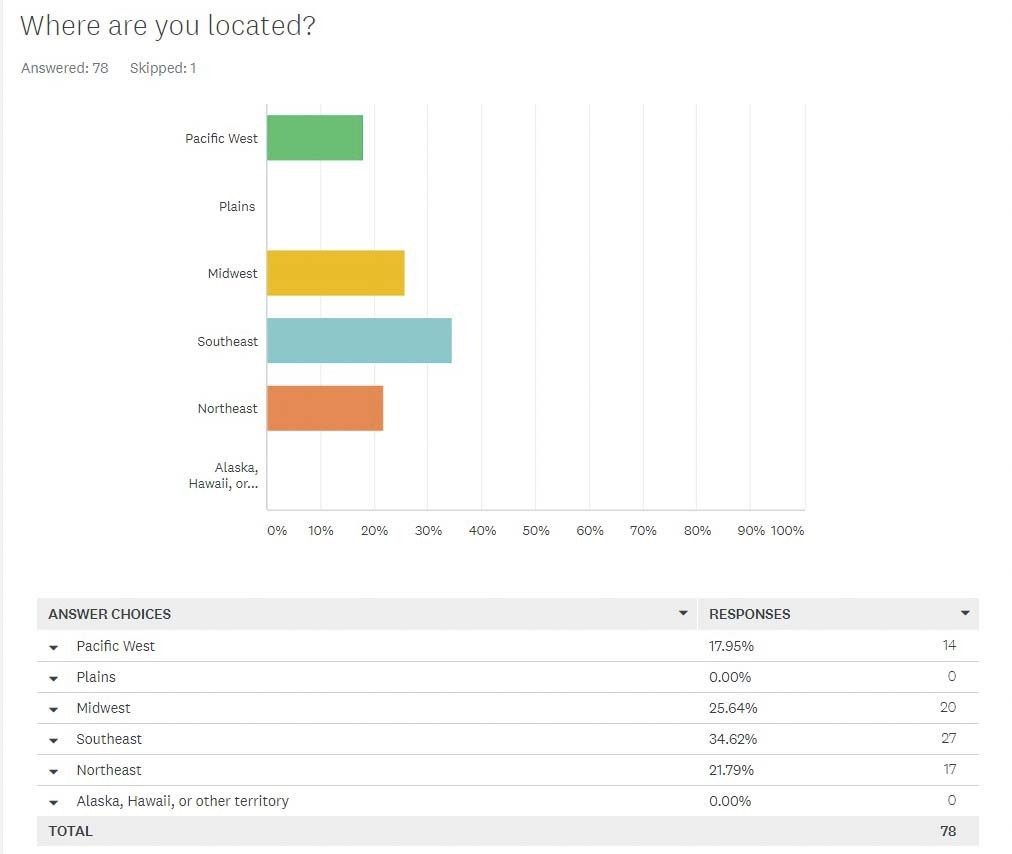
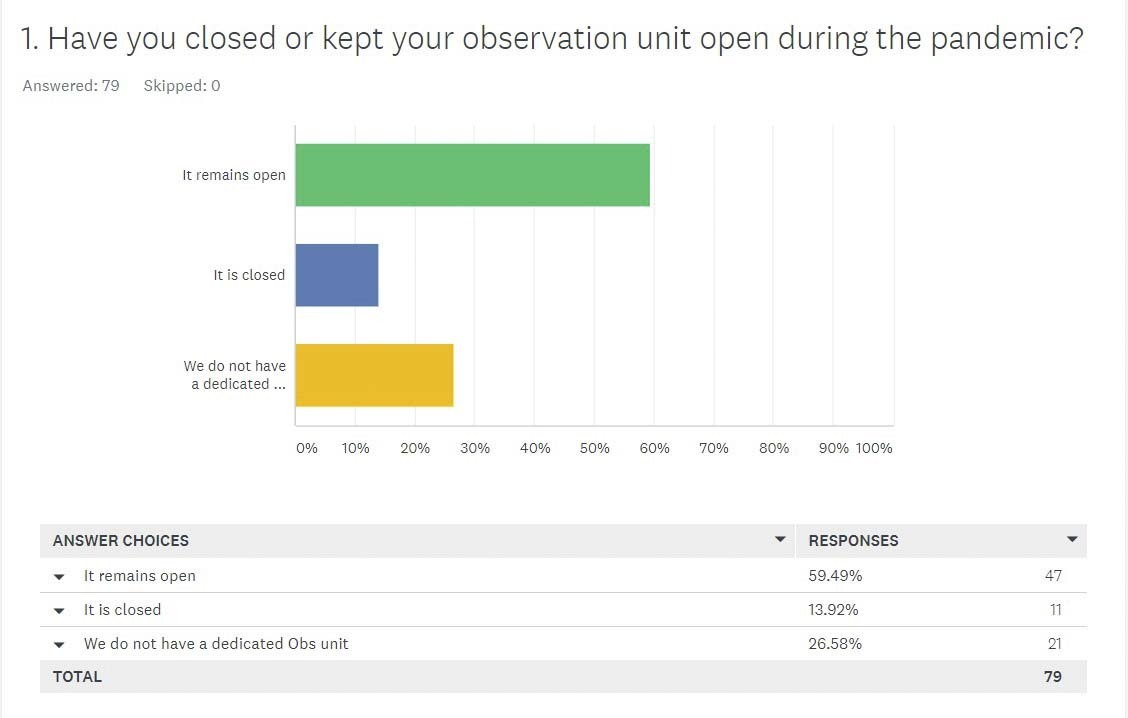
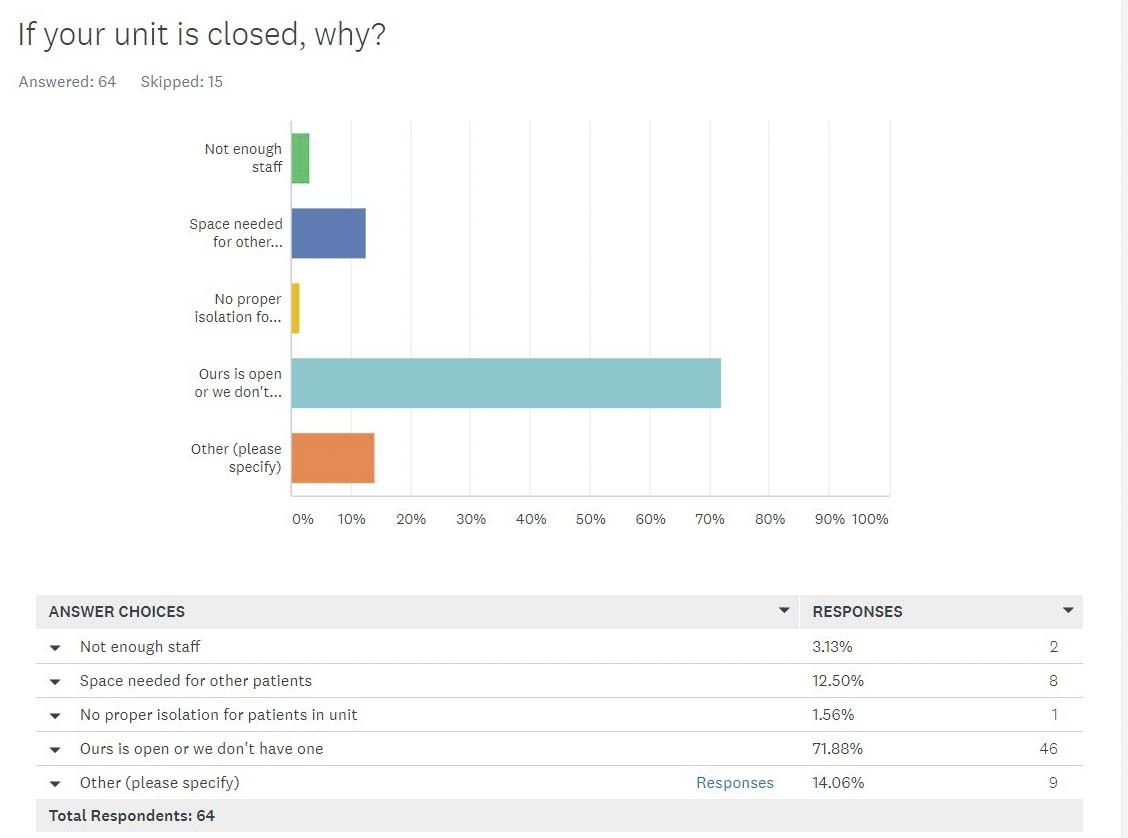
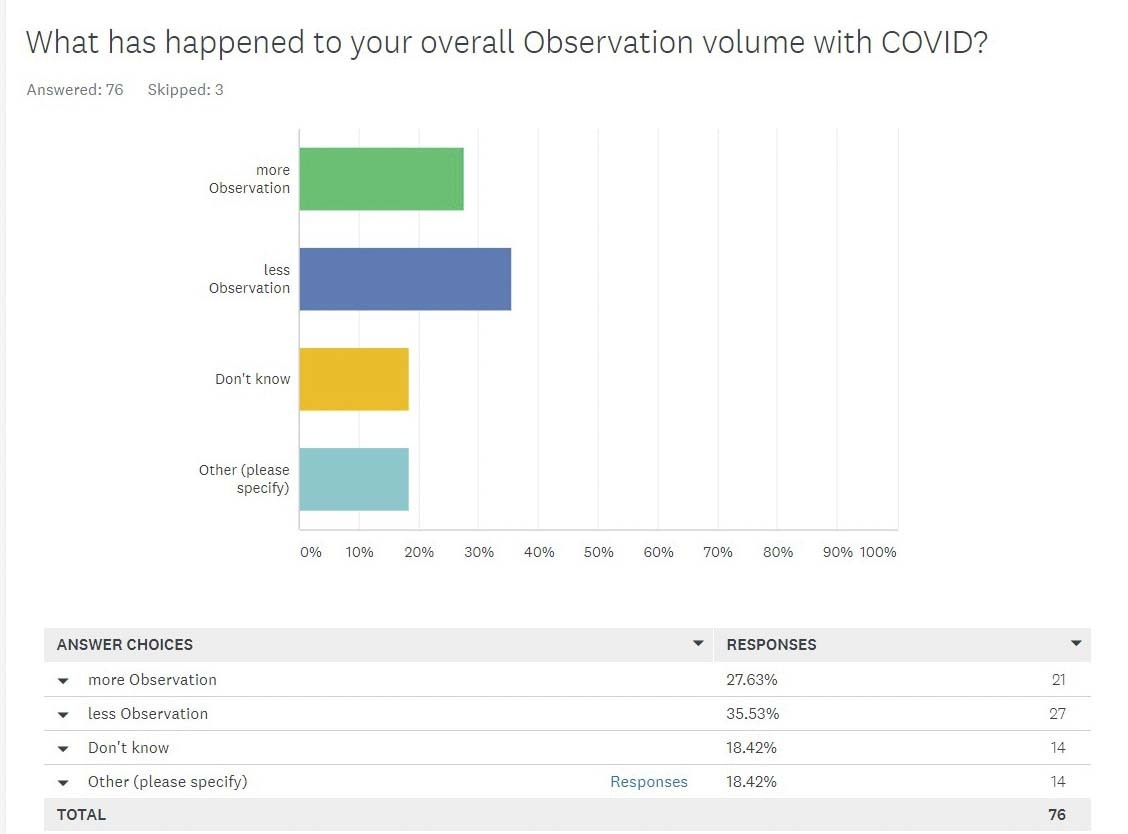
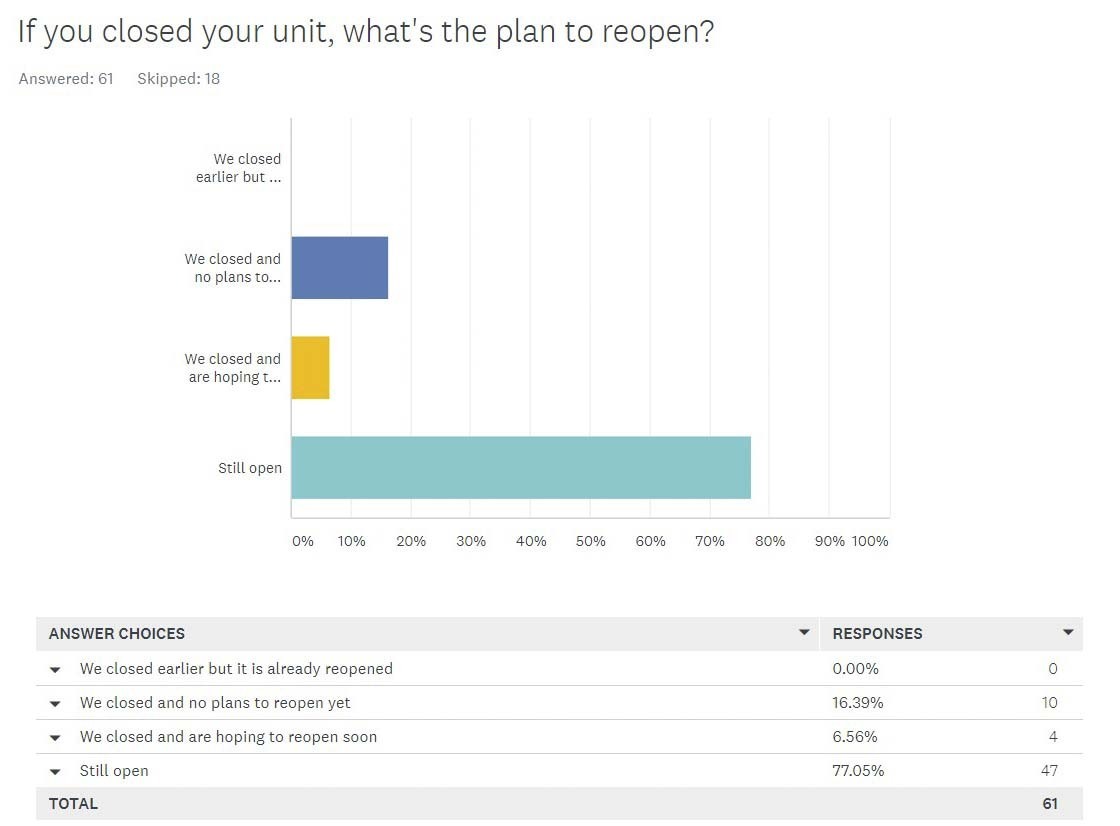
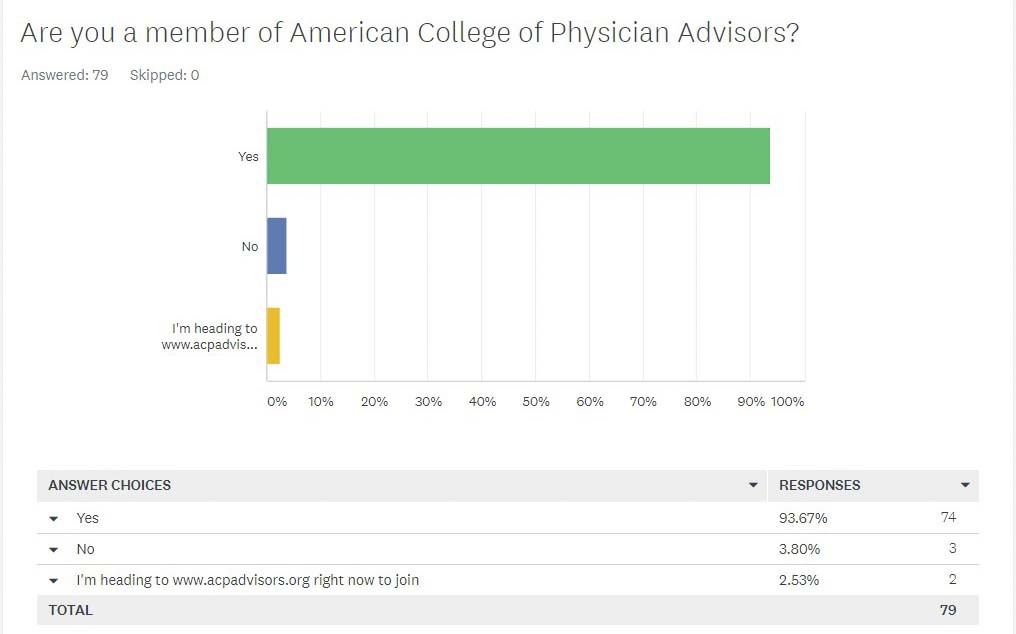
The purpose of this survey conducted by the American College of Physician Advisors (ACPA) was to determine the potential impact the SARS-CoV-2 pandemic may have had on dedicated Observation Units within hospitals. The survey was made publicly available online and was also distributed to individuals within the ACPA database. There were 79 respondents with 74 (93.7%) being members of the ACPA. Distribution of respondents skewed toward the East Coast (56.8%) and Midwest (25.6%). Of the 79 respondents, 58 (73.7%) had a dedicated Observation Unit within their affiliated hospital(s) and 21 (26.6%) did not have a dedicated unit. Of the 58 respondents associated with hospital(s) with dedicated Observation Units, 47 (81%) reported the unit remained open in 2020 during the SARS-CoV-2 pandemic whereas 11 (19%) closed. Among those that closed their Observation Units, reasons for closing included:
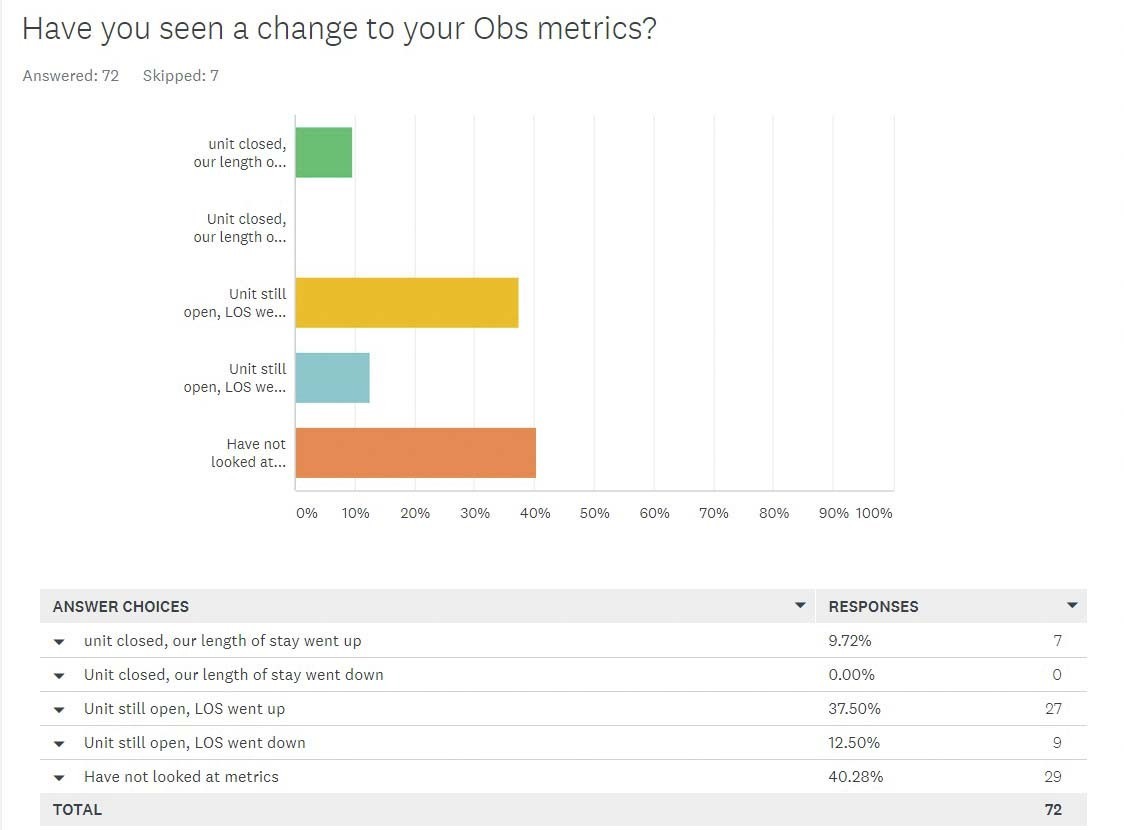
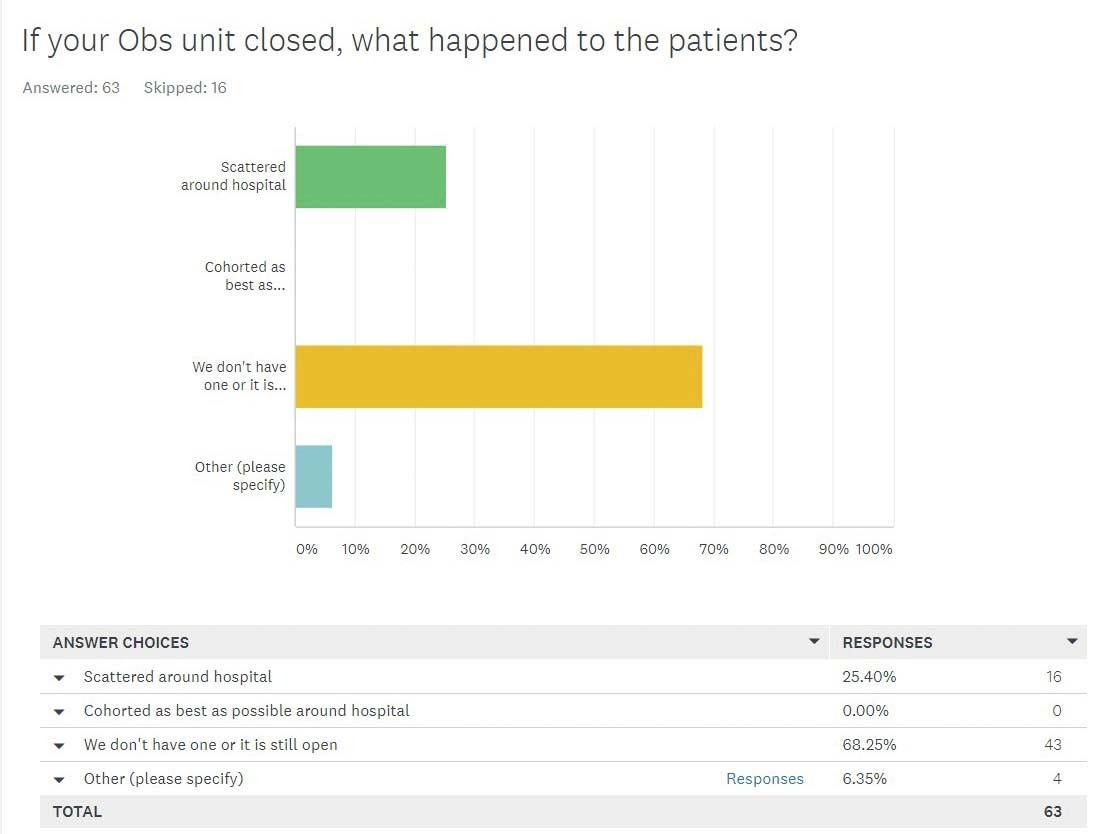
In the hospitals that closed their Observation Units, observation patients were most commonly reported as being scattered throughout the hospital (80%) vs. other, non-specified modalities of placement outside the closed unit. When asked whether length of stay (LOS) increased or decreased during 2020 with their Observation Unit remaining open vs. closed, 40.3% of the respondents were unable to provide data. However, the remaining cohort (59.7%) reported:
Conclusions 79 individuals representing hospitals or health systems responded to the ACPA survey on Observation Units during the 2020 SARS-CoV-2 pandemic. Of the 58 individuals reporting their hospitals had dedicated Observation Units, 81% of them reported the units remained open. 59.7% of the respondents knew about their facility’s LOS and of those, LOS was reported as higher in 2020 than in prior years 79.1% of the time whether the Observation Unit remained open or had closed. The most common reason cited for Observation Units closing in 2020 was reallocating beds to other (non-observation) patients. The survey was voluntary and resulted in a small denominator of respondents with a possibly even smaller representation of hospitals, given that multiple respondents might represent one hospital or collection of hospitals. However, given what is currently known about SARS-CoV-2 and that the preponderance of respondents to this survey kept their units open, Observation Units can potentially play an important role in future crises that result in an overwhelming surge of patients if advanced planning is conducted in 2021. Such planning should account for proper staffing, necessary equipment, and the establishment of practical infection control protocols for a high-turnover unit. Basic triage techniques as well as required intensity of service suggests that not all patients requiring hospitalization during a public health emergency need to be grouped together. It is our opinion that such practice leads to medical error. Observation Units can serve an important role in sorting patients into level of acuity of care needed in a very short period of time. Preparing 21st century Observation Units now, in advance of further disasters, will allow clinicians greater flexibility in how populations of patients are cared for when there is a wide range of ages and acuity within the population.
|