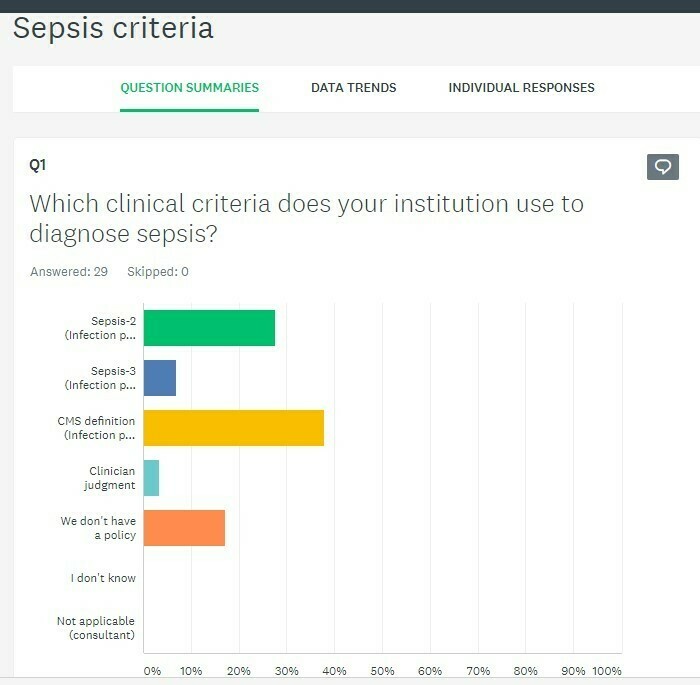
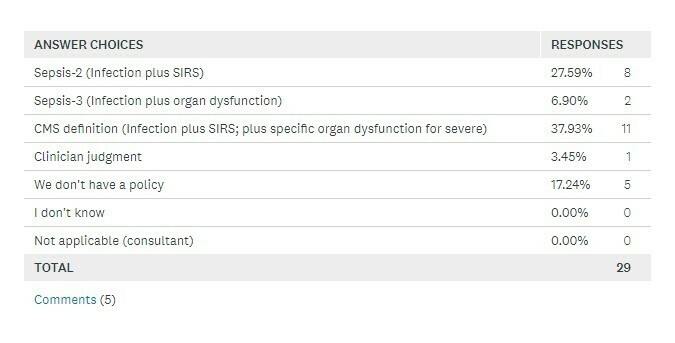
Caution: “Consensus”By Tim Brundage, MD, CCDS Consensus statements are not always consensus. I’m happy to report to the ACPA that our CDI committee is working very diligently on our sepsis education for the physician advisors. We enjoy creating material that we hope will provide value for the physician advisors who support our nations clinical practitioners. We were bestowed this honor by the ACPA, and we take it seriously. I am writing to respond to my good friend and colleague, Dr. Erica Remer’s article in the ACPA newsletter. I, along with many other physician advisors, value Erica’s opinion and I am happy that she shared it with the group. I am writing to clarify a few things that were shared. First, Erica is right that many physicians have chosen to adopt Sepsis-3 as their criteria for defining and diagnosing the condition. Our committee worked very hard on materials that were supportive of the article published in JAMA in 2016. We also made an effort to share the criteria for the SEP-1 core measure in our document (still in draft as of this writing). In addition, we had committee members who suggested the publication support physician advisors who are still using the Sepsis-2 criteria within their medical staffs. In an effort to determine who needed Sepsis-2 criteria material compared to those who needed Sepsis-3, we took a survey of our 42 member CDI committee. 29 of our members responded to our survey. The results are included.
Whether or not we like it there isn’t much consensus in sepsis. The Sepsis-3 “consensus” paper was authored by 19 physicians. I’m sure these 19 physicians are extremely talented and knowledgeable and well-studied, but this is still only the opinion of 19 physicians. (We have more physicians than that on our ACPA CDI committee) Honesty is a virtue. Honesty is what was published by the Surviving Sepsis Campaign of 2016 when they noted the quality of their evidence. Some of the evidence was honestly noted to be “weak”. The Surviving Sepsis Campaign of 2016 noted “Recommendations from these guidelines cannot replace the clinician’s decision-making capability.” It should also be pointed out that the Sepsis-3 publication noted that “sepsis is a syndrome without, at present, a validated criterion standard diagnostic test”. This ambiguity allows for the clinician to use his/her medical opinion when, and when not, to diagnosis sepsis. Erica and I had a wonderful discussion about “sicker than the average patient”. These words were in a draft version of our sepsis education. Dr. Ron Hirsch and Dr. Charles Locke both noted in their articles that patients with sepsis should be “sicker” or “very sick”. I agree, but this isn’t replicable. “Sick” to the family practice doctor may be different than “sick” to the critical care doctor. How would the reader know? As a committee we reviewed our survey and determined that education supporting the physician advisor practicing in the so-called Sepsis-2 hospital would need guidance, as would the physician advisor who is practicing in the Sepsis-3 hospital. As physician advisors in leadership roles in the ACPA we felt it necessary to provide both sets of supporting materials. The goal, of course, is to provide value to the doctors who work tirelessly to assist their clinical physician peers. I agree with Dr. Remer that our goal isn’t to be liked, but we need to take into account the committee works for the good of all of our members of the ACPA, especially when there is so little consensus in these so-called consensus documents. |